Great news!
Enhanced coverage for flash and continuous glucose monitors
We understand the challenges faced by those living with diabetes and recognize the substantial financial impact it brings.
Managing diabetes can be a lifelong endeavor, and may mean dealing with constant monitoring, requiring additional supplies and equipment.
Effective February 1, 2024, Flash Glucose Monitor (FGM) and Continuous Glucose Monitor (CGM) devices will have separate coverage limits under your plan.
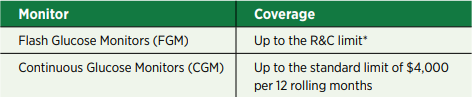
The new coverage limits are:
Eligible claims for each device, including CGM sensors, will continue to be submitted directly to Canada Life and paid from the healthcare plan. While CGMs remain subject to prior authorization, we recommend that you provide a cost estimate to Canada Life in advance of purchasing any new glucose monitor to confirm the amount eligible for reimbursement. Enhancing coverage for FGM and CGM devices is a positive step we can take in our ongoing support of your well-being and financial health.
Creating convenience: purchase sensors for your FGM device using your Drug Card!
We’re enabling a new level of convenience with your Drug Card and helping to simplify your health journey.
You can now easily purchase FGM sensors using your Drug Card at your preferred pharmacy.
That means you don’t need to submit a claim and then wait for reimbursement from Canada Life. However, you will still be responsible for paying any amounts over the R&C limits at the point of sale at your pharmacy.
*Reasonable and Customary (R&C) limits
Your CUPE EWBT plan covers customary charges for many services and supplies eligible under your plan. Our insurance providers determine the R&C limits, and ensure they are consistent with typical pricing in the area where treatment is provided.
If your service provider charges more than what’s customary, you’ll be responsible for paying the difference.
Making claims, made easier!
Fact: you may not need to be out-of-pocket for the full amount of an eligible plan expense while you wait for the claim to be reimbursed.
When your preferred health or dental provider is registered for eClaims through Canada Life, you get to enjoy point-of-sale submission of expenses. It relieves you of the hassle of paying for expenses out-of-pocket, then submitting a claim and waiting for reimbursement.
Canada Life’s Find a provider tool makes it easy for you to find out if your provider is registered (and remains eligible) to submit your eligible claims directly to Canada Life, so you don’t have to. And they update the list all the time!
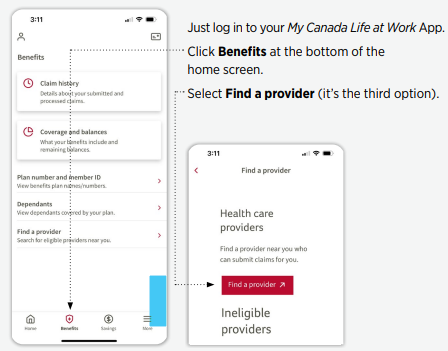
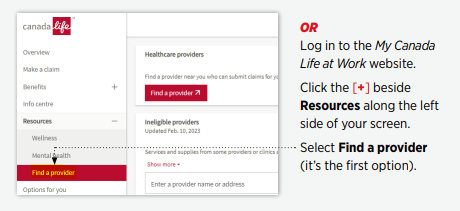
Just as important, you’ll find a list of Ineligible providers, too.
eClaims offers point-of-sale submission for registered, approved service providers – dentists, psychologists, massage therapists, chiropractors, optometrists, and others.
Canada Life’s efforts to expand the list of services available for eClaims registration means enhanced
flexibility and convenience for you, including:
- Chiropractors
- Physiotherapists
- Opticians
- Optometrists
- Naturopathic Doctors
- Massage Therapists
- Podiatrists
- Chiropodists
- Psychologists
- Speech Therapists
- Social Workers
- Occupational Therapists
- Osteopaths
- Psychotherapists
Canada Life can directly pay your approved provider the amount of your eligible claim that is eligible
for reimbursement; you’ll pay your provider any remaining balance. All providers must apply for approval to join the growing list of eligible eClaims providers.
Canada Life routinely reviews health care providers and clinics, and the claims submitted. If they don’t meet Canada Life’s requirements they are added to this list and Canada Life will no longer approve claims they’ve submitted.
Check back regularly, and continue simplifying your life.
Change in the prior authorization process for high-cost specialty drugs
Before the holidays we let you know that we would be introducing a new process to manage prescription drug prior authorizations for high-cost prescription drugs.
On January 1, 2024, Cubic Health, an independent third-party organization, began administering prior authorization for specialty prescription drugs. Previously, Canada Life managed the prior authorization process for specialty prescription drugs.
New prescriptions for drugs requiring prior authorization will be assessed through Cubic Health’s FACET Program (FACET) and its team of licensed clinical pharmacists. FACET is a member-focused program, designed to ensure that members receive independent and evidence-based assessments, quicker turnaround times for approvals (often within 24 to 48 hours), and that the most appropriate medication is prescribed.
March is Fraud Prevention Month
Fraud Prevention Month is an annual public awareness campaign held in March. The campaign is designed to keep Canadians from becoming victims of fraud, helping them recognize fraud attempts,
reject them, and report them.
Your CUPE EWBT benefits plan is affected by fraud, too. Fraudulent claims have a ripple effect on your benefits plan. When false claims are submitted, the entire plan suffers the consequences.
The pool of funds meant for legitimate claim reimbursements and opportunities to improve coverage is directly impacted. In the end, it’s our coworkers and friends who suffer, as money that could be used to pay for benefits is diverted to cover fraudulent claims instead.
We’re gearing up for the March campaign when we’ll share more information and tips to help you identify fraudulent activity and keep you – and all plan members – from falling victim to its effects.
Let’s work together to protect the integrity of your CUPE EWBT plan and ensure it continues to benefit us all for years to come.
Help keep us connected
When we can connect with you, we can continue to support and guide you toward becoming your
healthiest self – year-round.
It’s as easy as making sure your email on file with OTIP is current.
Want to check? Visit www.otip.com and update (or add) the email address you use most.
Want more information?
Need more information on your benefits? Or want to learn more about how the plan works? Check out the CUPE EWBT website at www.cupe-ewbt.ca. This is where you’ll find ongoing member updates, answers to frequently asked questions, the plan booklet and guide, as well as other useful resources.
For questions on enrollment and eligibility, you can call OTIP Benefits Services at 1-866-783-6847.
For questions on life, health, and dental claims, Canada Life’s dedicated CUPE EWBT line (1-866-800-8058) is here to help you.
And for any general inquiries or Trust-related issues, please email info@cupe-ewbt.ca



