Prior Authorization for Specialty Prescriptions
To help keep our plan sustainable and affordable, certain medications require prior authorization (pre-approval) before they can be covered. Learn below how to request prior authorization in a few simple steps.
What is Drug Prior Authorization?
Some prescriptions (such as medications with multiple uses or specialty drugs) require prior authorization (pre-approval) to be covered under the CUPE EWBT benefits plan.
Specialty drugs are used to treat complex, chronic or life-threatening medical conditions, and often have a higher cost.
Some of the more common conditions and medications requiring prior authorization include:
- Asthma/COPD
- Cancer
- Chronic migraines
- Crohn’s disease/ulcerative colitis
- High cholesterol
- Multiple sclerosis
- Psoriasis
- Rheumatoid arthritis
- Semaglutides (GLP-1)
If your prescription requires prior authorization, it cannot be covered by the CUPE EWBT benefits plan until it’s approved by our drug prior authorization partner: Cubic Health’s FACET team.
Cubic Health and the FACET Team

Cubic Health, an independent third-party organization, manages drug prior authorization for the CUPE EWBT benefits plan, through their FACET program and team of licensed clinical pharmacists.
Cubic Health and the FACET team are unbiased and have no financial incentive in their decision-making. A pharmacist – with expertise in the condition being treated – objectively assesses each medication based on cost-effectiveness and up-to-date evidence-based clinical criteria for the condition.
Confidentiality
The CUPE EWBT and your employer are never advised of your application, the FACET team’s decision, or any personal information you or your doctor provide to FACET. FACET communicates directly with you (or your dependent) and your doctor.
How to Know if a Drug Requires Prior Authorization
Your pharmacist should advise you (or your dependent) if prior authorization is required.
To learn whether the medication requires prior authorization before you go to the pharmacy, use Canada Life’s Drug Coverage Search Tool in My Claims to search for the name of your medication.
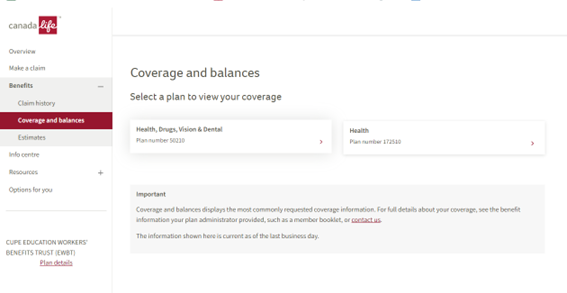
Click on Benefits and then Coverages and balances from the menu on the left side.
Select Health, Drugs, Vision & Dental (Policy number 50210).
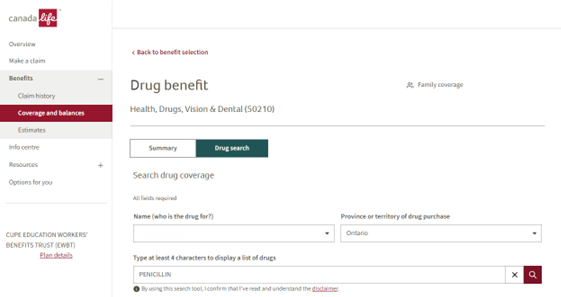
Select Drugs and then Drug search. Type in the name of the drug or drug identification number (DIN) and click Search.
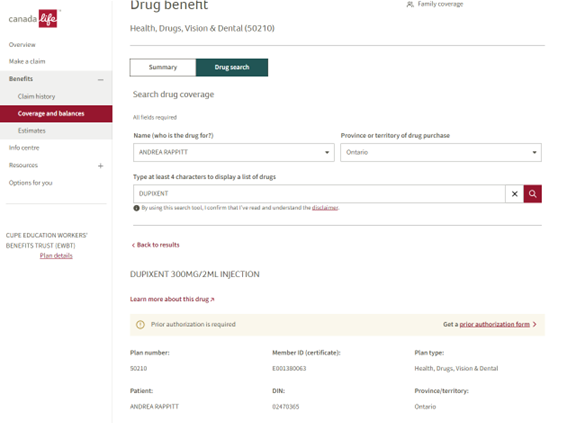
Choose the drug you have been prescribed to see whether prior authorization is required.
How to Request Prior Authorization
If Canada Life’s Drug Coverage Search Tool or your pharmacist indicates that your medication requires prior authorization, follow the steps below:
- Go to: www.facetprogram.ca/en
- Click on Find my form
- Search for the most applicable form based on your medication name
- Fill out the form with your physician and send it to FACET using the contact information outlined on the form. If your physician charges a fee to complete the form, this cost isn’t covered by the CUPE EWBT Benefits Plan.
FACET’s Decision
Typically the FACET team will communicate their decision (and their rationale) to you and your doctor within 2 business days after receiving all required information. A decision may take longer when additional information is needed.
If a drug cannot be approved, the FACET team will discuss alternatives with you and your doctor.
If a drug is approved (or conditionally approved), FACET will advise Canada Life. FACET approvals are valid for one year.
For more information about the FACET drug prior authorization program, view the Frequently Asked Questions (FAQs) on OTIP’s FACET site, or contact FACET.
Have Questions About Prior Authorization?
For more information about the FACET drug prior authorization program, view the Frequently Asked Questions (FAQs) on OTIP’s FACET site or contact FACET.