Our Journey Towards Better Well-Being: Balancing Care and Cost
Addressing the Trust’s financial situation, rising healthcare costs, and inflation while meeting members’ evolving needs is a delicate balancing act.
Over the past two years, we’ve made evidence-based adjustments and taken thoughtful steps to help control plan costs – and the need to do so continues. Our goal has been to minimize the impact of these changes on members wherever possible while upholding our commitment to providing benefits and support programs intentionally designed to enhance your well-being.

February
Enhanced access to care through expanded coverage for Nurse practitioners’ services
June
Introduced no-cost-to-you, expanded Starling Minds program, including mental fitness tools, and substance use and addiction support services.
September
Increase in Health and Dental member contributions – the first since plan inception
November
Cubic Health’s FACET Prior Authorization program for semaglutides, to help manage the rising costs of anti-obesity medications

January
Cubic Health’s FACET Prior Authorization program for high-cost specialty drugs
February
Enhanced coverage for CGM & FGM monitors
Enabled paying for FGM supplies with your Drug Card (lowering out-of-pocket expenses)
march
Fraud Education Campaign: protecting the integrity of our plan, together
april
EdvantagePerks passport to exclusive savings and deals
may
Enhanced drug management for specific weight-loss drugs
june
Increase in Health and Dental member contributions; decrease in Life premium rates
Change to Basic Dental and Dental scaling maximums

January
Medications used for weight management – be they glucagon-like peptide-1 (GLP-1) or others – will no longer be covered under the CUPE EWBT benefits plan
MemberRx: CUPE EWBT’s preferred specialty medications pharmacy
Together, There’s More We Can Do
You might already be familiar with the FACET Prior Authorization program, which has been providing CUPE EWBT members with access to specialty medications. You’ll see a change to the coverage of weight loss medications, and we’re introducing MemberRx – an innovative pharmacy designed to make managing your specialty medications even easier: it’s the best possible care while supporting the sustainability of your benefits plan.
Cubic Health’s FACET Program: Delivering Premium Care, Smart Savings
The CUPE EWBT began using Cubic Health’s FACET Prior Authorization program for complex specialty drugs at the beginning of this year.
Cubic Health, an independent third-party organization, manages drug prior authorization (pre- approvals) through its FACET Prior Authorization program. Their team of clinical pharmacists takes an evidence-based approach to reviewing prior authorization requests, with an intentional focus on patient care and outcomes.
Your FACET Clinical Pharmacist will:
- Objectively assess each medication request for a given condition, based on cost-effectiveness and current evidence-based clinical criteria;
- Determine whether the medication and dosage prescribed are the most appropriate;
- Reach out directly to you and your doctor for more information when needed;
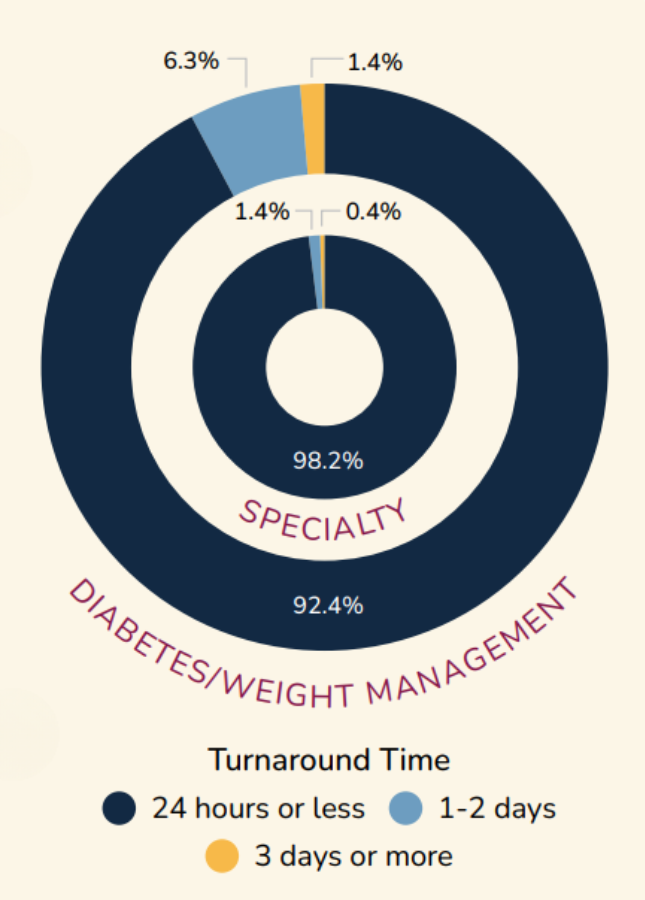
- Respond within 24 to 48 hours to both you and your doctor – and they stick to that promise!
You are also supported by a FACET Medication Access Coordinator (MAC) whose job is to help you understand your assessment and review the next steps.
It’s premium concierge care for you, designed to ensure our members receive the most appropriate, evidence-based treatment for their condition, and to protect the plan’s sustainability through smart financial management.
Cubic Health’s FACET Prior Authorization Program: Want to Know More?
Are you wondering which prescription drugs need to be pre-approved?
Or, how to submit a pre-approval (prior authorization) request?
Or, how the process to get your approval works?
It’s all here (on this website) and only a click away!
Update on Anti-Obesity Medications
Starting January 1, 2025, medications used for weight management – be they glucagon-like peptide-1 (GLP-1) or others – will no longer be covered under the CUPE EWBT benefits plan.
This means:
- Effective January 1, 2025, new prescriptions will not be approved for coverage;
- For members with an existing approved prescription, coverage will only continue up to April 30, 2025.
Several factors informed the difficult decision to eliminate this coverage:
- The demand and cost for anti-obesity drugs, including GLP-1 medications like Ozempic and Wegovy, as well as non-GLP-1 drugs like Contrave and Saxenda, have grown both rapidly and significantly in recent years and continue to do so, placing significant pressure on our CUPE EWBT plan.
- Many other benefit plans in the education sector already exclude coverage for these medications.
This step is necessary to ensure the plan remains financially viable, allowing us to continue offering comprehensive benefits to support all members and their families.
Optimizing Your Health, Enhancing The Care Experience
On January 1, 2025, MemberRx becomes the CUPE EWBT’s preferred pharmacy for certain
specialty medications.
Launched in 2023, MemberRx is a collaboration between OTIP (our plan administrator) and Cubic Health, the leading private-payer drug plan management company in Canada. MemberRx is Ontario’s first “plan sponsor pharmacy”, where dollars saved go right back into participating plans, helping to reduce their plan costs.
MemberRx innovates to provide comprehensive, high-quality, compassionate care – especially for plan members with complex health needs – to ensure better outcomes and overall health management. Unlike traditional pharmacies that prioritize profit, MemberRx operates without a profit motive, staying focused on what matters most: delivering the best possible health outcomes for you, and your loved ones.
Working hand-in-hand with the FACET Prior Authorization program, MemberRx simplifies the process for having your newly approved or renewing (already approved) specialty medications delivered. Along with prioritizing top-notch clinical care, they use drug-dispensing practices that help minimize the cost of providing coverage for high-cost specialty drugs – directly creating savings for our plan.
By using MemberRx, you are actively helping to reduce plan costs, supporting
the sustainability of the plan’s benefits. And that’s good for all.
MemberRx Fast Facts
- The CUPE EWBT is in good company as it joins other unionized education Trusts currently using MemberRx.
- MemberRx’s most recent patient survey revealed:
- Pharmacy care and sensitivity to patient preferences: 97% satisfaction
- An easy, seamless experience: 94% satisfaction
- Overall customer satisfaction: 92% satisfaction
- Their commitment to sustainability and eco-friendly practices is beyond compare: they offer no-cost packaging returns to enable reuse or recycling.
Using MemberRx is Easy: It’s Part Of The Facet Prior Authorization Program
Beginning January 1, 2025
FACET will automatically connect you with MemberRx to have your approved specialty drug prescription filled.

MemberRx will reach out to help you arrange free delivery of your prescription right to your door.
Do you, or your family members, have other specialty prescription medications you’d like filled? Before your prescription is dispensed, MemberRx will discuss your personalized health needs, including other specialty drug needs.
From initiating the prior authorization of your prescription medication to having it approved and delivered right to your door, it’s streamlined support to ensure an exceptional care experience.
Already Taking a Specialty Drug?
If you or your eligible dependant(s) are currently taking a specialty drug, your prescription can easily be transferred to MemberRx for fulfillment.
Just call 1-647-260-9797 and speak with a MemberRx pharmacy representative to have your specialty drug prescription transferred.
Be Prepared for Holiday Travel
- Download your digital Canada Life travel card to your phone’s wallet so it’s handy if you need it;
- Contact Canada Life and request a confirmation of coverage letter be emailed to you – it will include your name, plan, and certificate numbers; give it to a healthcare provider as proof of coverage in case of emergency.
Keep these details handy, too (in case your phone’s battery runs out!)
Global Excel Management 24/7 when you have a medical emergency while travelling:
- Canada or US: 1-855-222-4051 (toll-free)
- All other countries: 1-204-946-2577
(call collect, or include long-distance charges when submitting your claim)
Want More Information?
Reach out when you have questions – all providers’ contact information is on our website (at the links below).
Plan Enrolment, Eligibility & Premiums – OTIP Benefits Services
Health, Drug & Dental – Canada Life’s dedicated CUPE EWBT representatives are there for you
Travel Emergency Medical Assistance (Global Excel) – when you’re travelling outside Canada
Prescription Drug Prior Authorization – FACET (Cubic Health)
Preferred Pharmacy for Specialty Prescription Drugs – MemberRx
Life and AD&D Insurance Coverage, Claims & Conversion – OTIP and CHUBB Insurance
General inquiries or Trust-related issues
A final word
This bulletin has been prepared exclusively for eligible CUPE education workers in the province of Ontario covered by the CUPE Education Workers’ Benefits Trust. It is not intended to be comprehensive or provide advice. If there are any differences between the information provided in this bulletin and any legal documents that govern the delivery of benefits, the legal documents will apply. The CUPE EWBT Trustees have sole discretion to modify any or all plan terms, including benefits levels, eligibility conditions, premium share, limits and co-pay amounts.



