One of the most useful parts of your CUPE EWBT benefits plan is your dental benefits. Maintaining good oral health can help mitigate other health issues and is an important, yet often overlooked, part of your overall health.
As a member, your dental benefits coverage is quite robust.
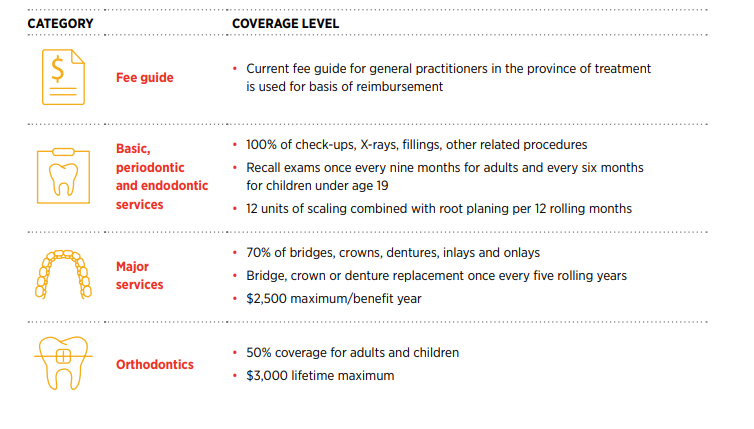
Here’s a quick summary of your coverage
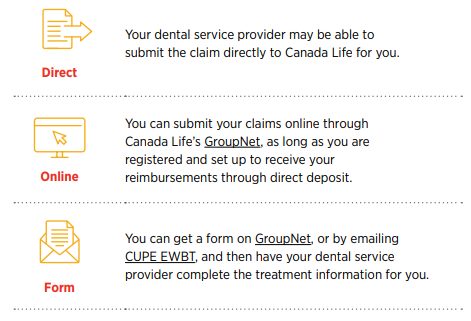
Submitting a dental claim is easy!
Making an informed choice
What your dentist charges for a service or treatment is their choice. However, that doesn’t mean that
your plan will cover whatever they charge.
Each province has a dental fee guide that is updated yearly and provides a suggested amount to dentists on what they should charge for services and treatments. In Ontario, dentists must tell their patients if they plan to charge more than what is suggested in the fee guide.
Insurers and benefits plans use these fee guides to determine the amount they cover. The CUPE EWBT benefits plan bases its coverage on the fee guide for the current year.
Planning ahead
Dental work can be expensive! Before incurring any large dental expense or beginning any orthodontic treatment, ask your dental provider to complete a treatment plan and submit it to Canada Life. The benefits payable for the proposed treatment will be calculated by Canada Life so you will know in advance of the approximate portion of the cost you will have to pay. A predetermination is essentially a cost estimate of the work needed. It’s useful to help you make more informed dental care decisions, since you can see the expected costs, how much you’ll be out of pocket, and if some of those out-of-pocket costs exist because your dentist charges more than the fee guide. It also helps smooth out the claims process and minimizes delays in being reimbursed.
What does this mean for you?
It means you should discuss costs and fees with your dental service provider. It could mean less money out of your pocket – and also helps the plan keep costs in check.
Important changes for members with a disability
Recently, the CUPE EWBT passed two motions that we feel will help members when they need it most. If you’re a member who is not enrolled in a long-term disability (LTD) plan, and you become disabled due to an illness or injury incurred while you are participating in this plan you can now:
- Access benefits at your usual contribution rate for up to 24 months.
- Access your benefits on a 100% member-paid basis.
The only caveat is that you must be approved for life waiver of premium.
Your employer will notify OTIP of your absence due to disability and OTIP will provide you with the necessary forms to apply for life waiver of premium with Canada Life.
We hope these changes help provide some peace of mind and support, if you ever need it.
End-of-year reminders
With the move to online classes and the new reality of dealing with a changing pandemic situation, this year has been unlike any other. Here are a few reminders as we get closer to the end of the year.
Statutory Leave – Emergency Leave policy
If there were a declared emergency/infectious disease emergency, rest assured you would continue to have access to your benefits at your current active rate until the leave is declared over.
Extension of coverage for overage dependents
In July, we announced this extension due to the COVID-19 pandemic.
At that time, if you had overage dependents that either reached age 21 and were not in school or reached the maximum age of 26, and did so after March 13, 2020, those dependents were granted an extension of coverage until August 31, 2020.
This extension applied to cancelled and rescheduled appointments or services that would have taken place had services not been interrupted by the pandemic.
All claims under this extension must be received by OTIP on or before December 31, 2020 in order to be eligible for assessment by Canada Life.
To make a claim under the extension, you will need to pay for services up-front then submit the claim for reimbursement. You must provide evidence that the service or appointment was cancelled or rescheduled by the practitioner during the March to August grace period, and your rescheduled appointment must have been completed by August 31, 2020.
If you have questions about reimbursement requirements or the proces for providing proof of these claims, contact OTIP at 1-866-783-6847.