How R&C limits affect COB
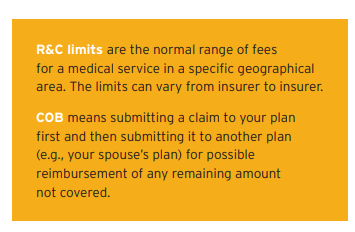
If you and your spouse both have health insurance, COB – submitting your claims to both plans – can be a helpful way to maximize your coverage. However, it’s important to remember that COB is also subject to R&C limits, which may vary depending on your insurer. So, while coordinating benefits may increase the amount of reimbursement you receive, the R&C limits may mean the claim is still not reimbursed at 100%.
How does it work?
Here are two examples…
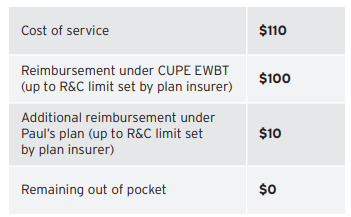
Example #1: Rebecca is a CUPE EWBT benefits plan member and therefore has an annual combined maximum of $1,500 coverage for physiotherapy, occupational therapy and athletic therapy. She recently visited her physiotherapist. The service costs $110– higher than the plan insurer’s R&C limit of $100. Rebecca also has $1,500 of physiotherapy coverage under her husband Paul’s plan, subject to his plan insurer’s R&C limit of $115 per treatment.
Assuming Rebecca hasn’t made any other physio, occupational therapy or athletic claims this benefit year, here’s how the reimbursement should work:
Example #2:
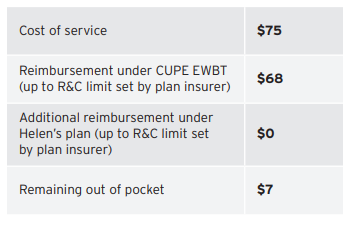
Mitch is a CUPE EWBT benefits plan member and therefore has an annual maximum of $500 for chiropractic treatment. Mitch’s practitioner charges $75 per treatment – higher than the plan
insurer’s R&C limit of $68 per treatment. He also has $500 of chiropractic coverage through his wife
Helen’s plan, and her plan insurer’s R&C limit is $60 for that service.
Assuming Mitch hasn’t made any other chiropractic claims this benefit year, here’s how the reimbursement should work:
Please note: Claims adjudication may vary based on insurer.
Some back to school reminders
As we start the new school year, here are a few benefit
reminders:
- Our benefit year runs from September 1 to August 31, so any benefit year limits – for example,
maximums for paramedical services like massage therapy or physiotherapy – will reset on September 1, 2019. - Your benefits coverage automatically continues from year to year, so you don’t need to re-enroll.
However, it’s important to notify OTIP, our plan administrator, if you experience an eligible life event (e.g., marriage/common-law, birth/adoption of a child, separation/divorce, death of spouse/
dependent child, spouse/dependent child becoming ineligible for coverage), in which case, you have 31 days to make changes to your benefits. - If you have a child who is over age 21 and enrolling in approved post-secondary education, you will have received an email from OTIP in June, as well as several reminders, to update his/her student status. If you did not log into the OTIP Secure Plan Member site and update your dependent(s) status, their coverage ended on August 31, 2019 (end of day), and you will need to call OTIP Benefit Services at 1-866-783-6847 right away to have them reinstated.
- If you have any outstanding claims to submit for the benefit year ending August 31, 2019, you have 6 months for online health or dental claims, and 15 months for paper claims. In case of termination of coverage, you have 180 days from your termination date to submit any outstanding claims.
Fall benefits checkpoint
Remember, in October, there will be a “checkpoint” to update any changes to your hours that may affect your eligibility and/or premium share going forward for 2019-2020. Any premium changes identified during the October checkpoint will come into effect in November.
If your regularly scheduled hours have decreased as of the October checkpoint, you will move to the appropriate category, and your premium share will be adjusted accordingly. If your regularly scheduled hours increase during the year, you will be able to take advantage of the lower premium share and will not have to provide medical evidence of insurability for health and/or dental coverage, if you apply for coverage within 31 days of the increase.
If you have a decrease in hours that affects your benefits funding level, your benefits will be suspended effective November 1st. You will be sent an email by OTIP to complete an event and reinstate the benefits that you wish to continue. This ensures that the higher level of premium required for your benefits is not deducted from your bank account without your permission.
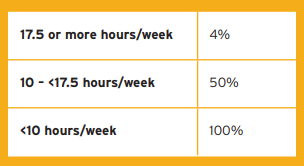
As a reminder, benefits cost-sharing for Health and/or Dental falls into three categories:
A closer look at benefits fraud
Benefits fraud has been getting a lot of attention in the media recently – and for good reason. It’s a serious issue that costs plans money.
Fraud can take many forms, such as:
- Purposely providing false information or withholding information to ensure a claim will be paid;
- Receiving medical items or services that you might not need for a monetary or material benefit;
- Unlicensed providers performing services, or licensed providers performing services outside of their licensing/scope of practice;
- “Upcoding” (claiming a more expensive procedure than was actually done); and Providers billing for services not actually rendered, members making claims for services they did not receive, or inflating the cost or amount of those services.
Here are some tips to combat benefits fraud:
- Don’t change dates on claims or withhold any information;
- Ensure the claims you submit are for medically necessary supplies and services, and don’t accept receipts for any services or supplies you haven’t received;
- Be cautious of practitioners that offer “gifts” or refer you to another provider for a prescription;
- Don’t provide blank, signed forms to a service provider to submit a claim later on your behalf; and
- Know who you’ve given your benefits information to, and what forms you’ve signed.
Why does all this matter?
Because benefits fraud impacts the financial health of our plan and increases the costs of running it. Ultimately, this may lead to added costs for you and your fellow members, or benefits reductions to ensure plan sustainability. Members who are personally involved may face fines or loss of coverage.



